FAQ
Status: 03/09/2023 07:01
So far, little has been done digitally in the healthcare sector. Paper and a fax machine are often the means of choice. Minister Lauterbach now wants to promote electronic patient records. This offers advantages – but also harbors risks.
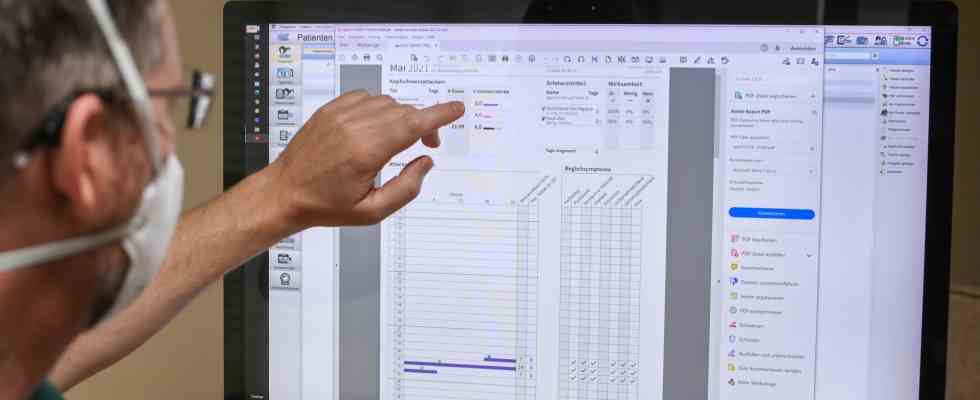
X-rays on CD, doctor’s letters on paper, findings by fax – digitization doesn’t seem to have arrived in the healthcare sector yet. Federal Minister of Health Karl Lauterbach (SPD) wants to change that and is pushing ahead with electronic patient files. Every health insured person should therefore receive an electronic patient file in the next year. It offers many advantages. It could prevent dangerous drug interactions, for example. But there are also risks, for example in data protection. An overview:
What is the status quo?
Since the beginning of 2021, all 74 million people with statutory health insurance have been able to receive an electronic patient record (ePA) from their health insurance company. The so-called opt-in rule applies, i.e. use is voluntary. The insured decide for themselves whether and how they use the file. This was laid down in the Appointment Service and Supply Act, which the former Federal Health Minister Jens Spahn (CDU) had introduced. Resident doctors and hospitals must therefore be equipped with all the necessary components to use and fill in the electronic patient file.
For patients, this means: They have to take care of themselves if they want to use the EHR. To do this, they have to download an app from their health insurance company and register with their health insurance company to use it. The patient file must then be activated, for example with the electronic health card and a PIN. Documents such as doctor’s letters, laboratory values and findings can then be saved in the file. If they are not yet digitized, that means: scan and upload.
What is the problem so far?
Less than one percent of patients currently use the electronic patient file. Many do not know anything about it, for others the registration and application is too time-consuming. In addition, the design is subject to criticism. Doctors speak of a hodgepodge of pdf files with no structure. According to Stiftung Warentest, not everything runs smoothly when setting up, navigating and managing documents. Three ePA apps from three health insurance companies were tested for this. The conclusion: the path to the digital file is “still bumpy and requires a lot of patience”.
So far, the electronic patient file has not been a success story. This is also illustrated by the sluggish process leading up to the introduction. Because the idea is already 20 years old. As early as 2003, the then Health Minister Ulla Schmidt (SPD) launched an electronic health card. There are many reasons for the long delays. Initially, associations of doctors, health insurance companies, pharmacists and clinics were tasked with advancing the project. But in the company “Gematik”, which was founded especially for this purpose, conflicts and blockades accumulated. There were also technical problems and discussions about data security.
Electronic medical records will become mandatory at the end of 2024
Nadine Bader, ARD Berlin, daily news at 8:00 p.m., March 4th, 2023
What is Lauterbach planning?
The Federal Minister of Health wants to fundamentally change the procedure. In the “Frankfurter Allgemeine Sonntagszeitung”, Lauterbach announced a new, more binding procedure for the end of 2024, the so-called opt-out procedure. Anyone who does not expressly object should be included automatically. It should also be available to patients who do not wish to set up the electronic file themselves. Doctors could then use the file to exchange information, for example. Even if the insured do not download an appropriate app and do not actively agree to its use. The SPD, Greens and FDP had agreed on this procedure in the coalition agreement.
Lauterbach also wants to facilitate the use of health data for medical research. Otherwise, Germany will soon no longer play a role in pharmaceutical research. There is already a lot of data, but it would be stored separately, for example in the hospitals, with the health insurance companies and the cancer register. It should be possible to combine this data in pseudonymised form for research purposes. Pseudonymized means that the name and other identifiers are replaced by an identifier.
Janosch Dahmen, the health policy spokesman for the Greens, also sees this as an advantage. This hides the concrete identity. Nevertheless, this would make it possible to conduct research for specific groups, for example genders or children.
How would patients benefit?
The advantage for medical professionals is obvious. A functioning electronic patient record would quickly provide information about what medication a patient is taking, what previous illnesses they have, what examinations were carried out beforehand and how previous treatments went. Much of this information is currently distributed in the various medical practices and hospitals.
They could be vital in an emergency, for example if doctors in the emergency room could simply access the patient’s medical history digitally, says Christian Karagiannidis, President of the German Society for Internal Intensive Care and Emergency Medicine. In order to strengthen trust in the file, health politician Dahmen advocates that sensitive health information can only be viewed in stages. A “shadowing” of ePA content would mean that certain information would only be available to selected treating physicians.
The Advisory Council on the Assessment of Developments in the Health Care System also considers it sensible to allow the insured to make such a gradation. The Council had already spoken out in favor of the opt-out procedure in 2021. An electronic patient file should be set up for each person at birth. The council argues: sharing data means better healing. On the one hand, the experts expect a more targeted therapy for the patients. On the other hand advantages for research. They recommend forwarding the treatment data in pseudonymised form to a central “collecting point”, a research data center, which manages and saves this data and makes it available for research purposes.
What concerns are there?
There is a risk that the data will fall into the wrong hands and this could have serious consequences if used improperly. For example, social stigmatization or discrimination for the people concerned, for example in the labor and insurance markets.
The Central Ethics Committee at the German Medical Association therefore recently called for suitable transparency and supervisory structures that ensure data security and compliance with ethical standards. In any case, the introduction of an opt-out solution must be accompanied by a broad social debate and comprehensive information for the population.
According to Lauterbach’s plans, the fact that patients no longer have to actively consent to the use of their data goes too far for the German Foundation for Patient Protection. “The electronic patient record makes sense and is correct,” says Eugen Brysch from the foundation. However, the file should not undermine patient rights. Silence is never consent, that applies to data as well as to medical interventions. However, the opt-out regulation would probably be possible under data protection law, depending on the design. The German Medical Association refers to the General Data Protection Regulation. According to this, the processing of particularly sensitive personal data such as health data is only permissible on the basis of the consent of the person concerned or on the basis of a law. Such a law would have to get Lauterbach on the way.
What does the Federal Data Protection Commissioner say about this?
Little so far. Ulrich Kelber is holding back in the debate. On request from the ARD Capital Studio lets Kelber say that he is currently not available for an interview on this topic. It is unclear whether this indicates differences with the minister’s plans or whether Kelber wants to wait for the precise legal form of the project. Most recently, the Federal Data Protection Commissioner was critical of the intended procedure of only dispensing with the file if patients actively object.
In November 2022, Kelber told the Berlin “Tagesspiegel” that, in terms of data protection policy, switching to an opt-out would not be a good idea if you wanted the public’s trust. He complained that many areas of application were still missing, in particular structured data, emergency files and medication plans and, at the beginning, basic functionalities for data protection. Trust in the digitization of the healthcare sector is not strengthened in this way.
In the so-called Petersberg declaration on data protection-compliant processing of health data in scientific research in November 2022, the data protection officers of the federal and state governments called for a legal basis. Encryption, pseudonymisation by a trustee or the earliest possible anonymisation of the data were mentioned as basic guarantees and measures. In addition, further requirements would have to be placed on the procedure and the implementation of the research.