Today Parliament is deciding on one of Health Minister Lauterbach’s most important projects: from 2025 everyone should have an electronic patient file. Critics say the plans go far too far.
When a patient is taken to the hospital in an ambulance, every minute can count. Important information is often missing: Are there any previous illnesses or allergies? What medications is the patient taking? Until now, doctors have had to laboriously collect this information.
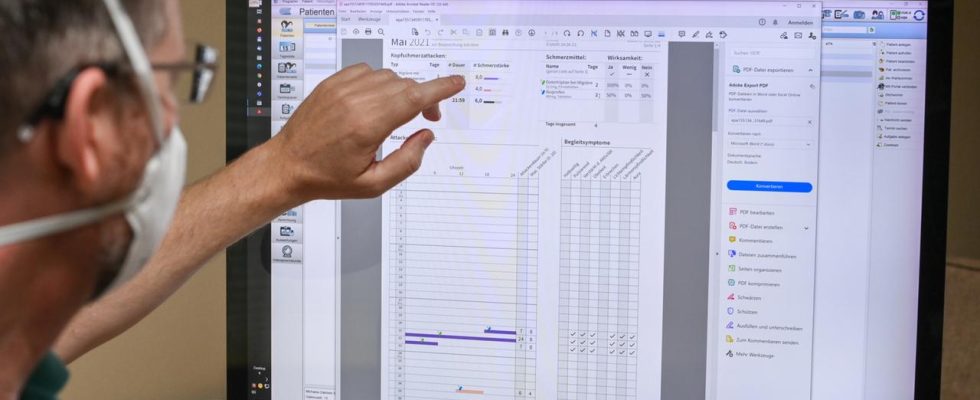
Intensive care physician Christian Karagiannidis knows this all too well from his everyday hospital life. Someone from the team has to make calls and organize preliminary findings. If things are going well, practices send a fax. When things are going badly, there is no one to reach. The emergency team is then on hold. Important time is lost. That’s why Karagiannidis is hoping for the electronic patient record (ePA). He says the file could save lives. Especially when patients are no longer responsive in an emergency situation.
Digital files have so far only been used by one percent
The electronic patient file is the heart of the digital laws of Health Minister Karl Lauterbach, who promises a “catch-up” in digitalization. So far, the digital file has been used by around one percent of patients. This is also because the insured persons have to take care of activating the ePA themselves. In addition, registration is complicated and there are not that many functions.
That should change. From 2025 everyone will automatically receive a digital file – unless they actively object. This procedure is called “opt-out”. The statutory health insurance companies are responsible for this. Private health insurance companies can also offer their insured persons a patient file, but they are not obliged to do so.
From Medication schedule to track fitness
Patients should be able to decide for themselves which data ends up in the file and who is allowed to see it. Even in the year after next, the ePA will by no means offer all the functions that the insured want. The file will be developed further over time.
X-rays or MRI images will probably not be saved in the file initially, but only the corresponding findings. In the first step, for example, all medications will be stored in a digital medication plan. This allows doctors to get a better overview in order to avoid dangerous drug interactions.
But not only doctors can fill out the ePA. If you want, you can also feed it with data from fitness trackers or smartwatches, for example. An interface to the organ donation register is also planned, which is scheduled to start next year. Legal guardians can manage the files of their children up to the age of 15 and anyone who looks after their parents in need of care should also be able to access their data. If you don’t have a smartphone or computer, you can get help at the pharmacy or at the health insurance company’s ombudsman offices.
Patient advocates are skeptical
If someone doesn’t comment at all, a digital file is automatically created. Patient advocates have fundamental concerns about this. They want you to still have to actively consent to receive an electronic patient record. Another point of criticism: Sensitive data such as the treatment of mental illnesses should also generally be included in the file. However, doctors are then obliged to point out that the processing of the data can be restricted. In addition to mental illnesses, this also applies to sexually transmitted infections and abortions.
From the point of view of Federal Data Protection Commissioner Ulrich Kelber, this is not enough. The concern: Patients could be overwhelmed because they are under stress. For example during psychological treatment. From the Federal Data Protection Commissioner’s point of view, this could mean that insured persons do not make the same decision as they would without time pressure and with advice from people they trust. As a result, data could end up in the ePA, which could lead to discrimination and stigmatization of the insured, Kelber fears.
For traffic light health politicians, however, another aspect is more crucial. They say: Such sensitive data is also relevant and should be included in the ePA. For example, because some medications for depression can trigger cardiac arrhythmias. This information can be crucial for the treating cardiologist. From the perspective of Green health politician Janosch Dahmen, it would be dangerous to implement the ePA as suggested by the Federal Data Protection Commissioner.
Organizations are demanding more transparency
The Federal Minister of Health has set the goal of around 80 percent using the ePA by the end of the year after next. This will only work if the benefits of the record outweigh the benefits for people and they trust that their sensitive health data is truly secure.
This is exactly what an alliance of several organizations, including the German Aids Aid, the Federal Association of Consumer Organizations and the AG Kritis, doubts. They have expressed themselves in an open letter and, among other things, are calling for more transparency. Manuel Atug, spokesman for AG Kritis, does not believe that the digital laws provide sufficient security. He assumes that large data sets are being intercepted illegally. “We have already seen this several times internationally, that millions of health data have been published. This threatens us in Germany in concrete terms and not just in theory.” Atug fears that German health data will also be stolen on a large scale in the next five to ten years if the government does not improve the law again.
Christine Aschenberg-Dugnus, FDP health politician, believes it is unlikely that the data will be stolen. Of course, there is no absolute security. “If you have reservations, you have to decide for yourself what is more important: designing everyday care well or the theoretical possibility that the data might end up in the wrong hands.”
High time expenditure for the health insurance companies
The health insurance companies consider the schedule for the ePA too ambitious. They must make the file available to everyone and educate their insured persons so that they can make a decision for or against the ePA. No binding legal basis will come into force before February 2024, says the CEO of the National Association of Statutory Health Insurance Funds, Doris Pfeiffer. Therefore, the ePA should not start for everyone until July 2025, i.e. six months later.
There is also a dispute over who should transfer the numerous older medical documents into the file. It could be relevant for patients that older documents subsequently end up in the digital file. The health insurance companies don’t want to do that. And it is unlikely that doctors will have time for this. You will already be busy supplying the ePA with the latest data.
Pilsinger: “Oligopoly of manufacturers”
In order for the ePA to be a success, it actually depends on not only the patients taking part, but also the doctors filling out the file. The CSU health politician and doctor Stephan Pilsinger is worried that the technical details could end up causing problems for practices.
In addition to his work as a member of the Bundestag, he works in a family doctor’s practice. There are always difficulties with the practice management system. The patient’s findings and diagnoses are stored there. Some of the systems are outdated. Doctors can’t just change them. Transferring patient data to newer systems does not work or is associated with high costs. Pilsinger speaks of an “oligopoly of manufacturers”. He says: The federal government should regulate more here, i.e. give manufacturers guidelines so that doctors can switch to newer systems more easily.
Data could be used for research
The digital laws are also intended to help make Germany’s role as a research location more attractive again. Lauterbach wants to make it easier for scientists and pharmaceutical companies to use pseudonymized health data for their research. To do this, databases that already exist should also be accessed, such as the cancer registry, data from health insurance companies and hospitals. In the future, data from the electronic patient file will also be included. Anyone who does not want their data to be used for research must actively object.