NHS patients should be able to pay to access care faster, Sir Tony Blair has urged.
On the health service’s 75th birthday, the former Prime Minister warned it may not survive another five years without a ‘fundamental reform’.
He claimed letting Brits fork out to skip record queues could help the ailing system thrive.
Options to ‘co-pay’ for treatment that is approved in the UK but the NHS would not normally fund may also ease unsustainable pressure, Sir Tony said.
Labour also warned today that the NHS ‘will die’ without urgent changes.
Health Secretary Steve Barclay today admitted the health service, which gets in the region of £150billion-a-year, needs to adapt.
However, he said this should stem from a gradual change rather than the ‘big bang’ critics have demanded and insisted that the Government is ‘fully committed’ to the founding principle of it being ‘free at the point of use’.
It comes as a minister today admitted that the record NHS backlog, which currently stands at 7.4million people, is only set to keep growing.
Knock-on effects of Covid and lockdowns, never-ending strikes and a staffing crisis have heaped huge pressure on hospitals.
The number of people waiting for routine hospital treatment in England soared to a record 7.42million (red line) in April, figures show. More than 370,000 people in the queue for routine ops, such as hip replacements, were waiting for more than a year (yellow bars)
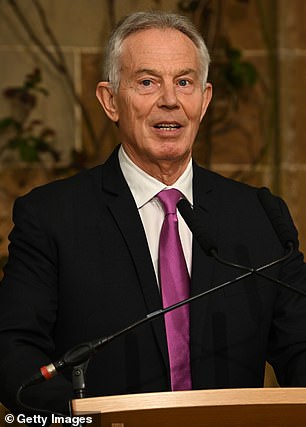
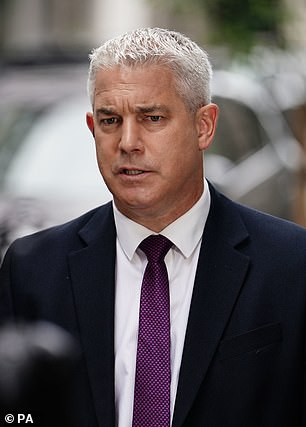
There should also be the option to ‘co-pay’ for treatment that is approved in the UK but the health service would not normally fund, Sir Tony Blair (left) recommended, warning that the NHS is unlikely to see its 80th birthday without radical reform. Health Secretary Steve Barclay (right) today admitted that the health service needs to adapt but said this should be a gradual change rather than a ‘big bang’.
In a report by the Tony Blair Institute, the former Labour leader said while the NHS is based on the principle of free care for all, the number of Brits going private has ‘rocketed’ in recent years as the service struggled to provide timely care.
He blamed this on Brits facing long waiting lists, difficulties seeing their GP and the ‘complicated and inefficient’ process to access care.
As a result, Sir Tony called for an NHS overhaul, including working with more private providers and partners to introduce ‘co-payment options’ that allow Brits to pay to access treatment faster or ‘co-pay’ towards care that is approved by the NHS, but it would not usually fund.
He warned that the health service is ‘unresponsive’ to the digital transformation, the workforce is overstretched and morale is poor.
It is ‘unlikely the NHS will survive to see its 80th birthday’ without proper investment and a ‘firm commitment to reform’, he added.
Sir Tony’s other recommendations include every Brit have their own personal health account on the NHS App, which is ‘owned by the patient not the service’.
It would include their health data from smartwatches, self-testing and diagnosis that, with patient permission, can be accessed by the NHS and private companies.
Additionally, patients should be able to access ‘a lot of basic care’ more easily through pharmacies, at work, in gyms and supermarkets.
Using technology to do or help with NHS work, hiring more digital experts and expanding the use of whole-genome sequencing were among Sir Tony’s other recommendations.
While the Health Secretary today acknowledged that the NHS needs to change and adapt to improving technology and medical advancements, he said this should be a ‘constant evolution — not a big bang moment’.
Writing in The Times, Mr Barclay added: ‘But equally, in order to keep improving care for patients and providing value for money for taxpayers, we’ve made clear the NHS needs to continue to reform.
‘That has been a key message of this Government, as shown by our shift to modern methods of construction in our new hospitals programme, backed by over £20billion.
‘It also includes the publication of the NHS Long-Term Workforce Plan last week — the first of its kind in the history of the NHS.
‘Backed by over £2.4billion, it sets out how the NHS will address existing vacancies and meet new challenges by recruiting and retaining hundreds of thousands more staff over the next 15 years, as well as modernising and reforming the way they work.’
Staffing shortages throughout the health service — which has around 150,000 vacancies — have been blamed for long waits for care, the overstretched workforce and staff burnout.
The blueprint, unveiled by the Prime Minister last week, detailed the ‘most ambitions plan in NHS history’ to tackle the crisis by slashing waiting lists and boosting the NHS workforce with 60,000 more doctors and an extra 170,000 nurses by 2036/37.
Bosses also expect to have an additional 71,000 allied health professionals such as physiotherapists, midwives and pharmacists.
It comes after former Health Secretary Sajid Javid yesterday called for an overhaul of the NHS, describing the service as ‘frozen in time’.
Mr Javid said that the current structure of the NHS has left Brits sicker than those in many other Western countries, with the UK having lower life expectancy and cancer survival.
The MP for Bromsgrove said both major political parties privately believe the NHS is ‘unsustainable’ in its current form and will be unable to cope with surging demand, despite record levels of funding.
But Mr Barclay disputed this — writing that ‘colleagues across Government’ are ‘fully committed’ to the NHS founding principle of ‘free at the point of care’.
‘I’m confident that with our plans for recovery and reform and an embrace of technology and innovation, it will be fit to deliver the best care to patients for another 75 years,’ he said.
Shadow Health Secretary Wes Streeting, who has backed using the private sector to bolster the NHS, echoed calls for reform to make the service sustainable for the long term.
He told Times Radio: ‘We’ve got to shift the focus of care from hospital into the wider community, fix the front door to the NHS in general practice, more care and support for in people’s homes.
‘We’ve got to shift the system from being an analogue system to one that’s more digitally-driven and able to harness the enormous opportunities from life sciences and technology that we have in this country.
‘And thirdly, we’ve got to — in a broader sense, beyond the NHS — focus on preventing ill health, promoting good health.’
He added: ‘If we have those three big shifts, we will have an NHS that’s fit for the future, free at the point of use, there for us when we need it.
‘But that’s a far cry from where we are today, where we’ve got the absurd spectacle of ministers celebrating the 75th anniversary of an institution that they have broken.’
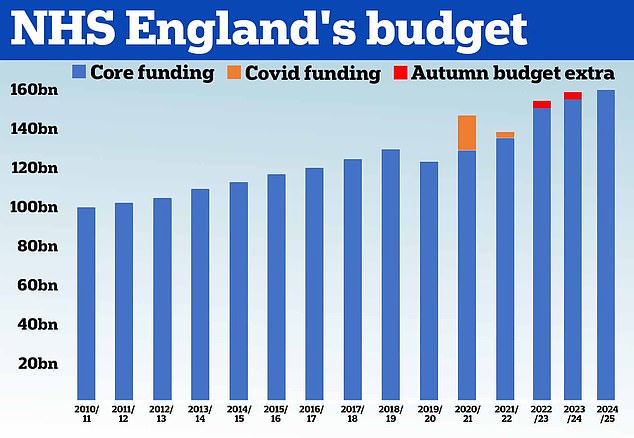
NHS funding is has risen sharply in recent years, with a total budget of £152.6 billion in 2022/23, some £28.4 billion more than in 2016/17 at 2022/23 prices. The graph does not reflect the extra £2.4billion pledged by the Government in its long-term workforce plan
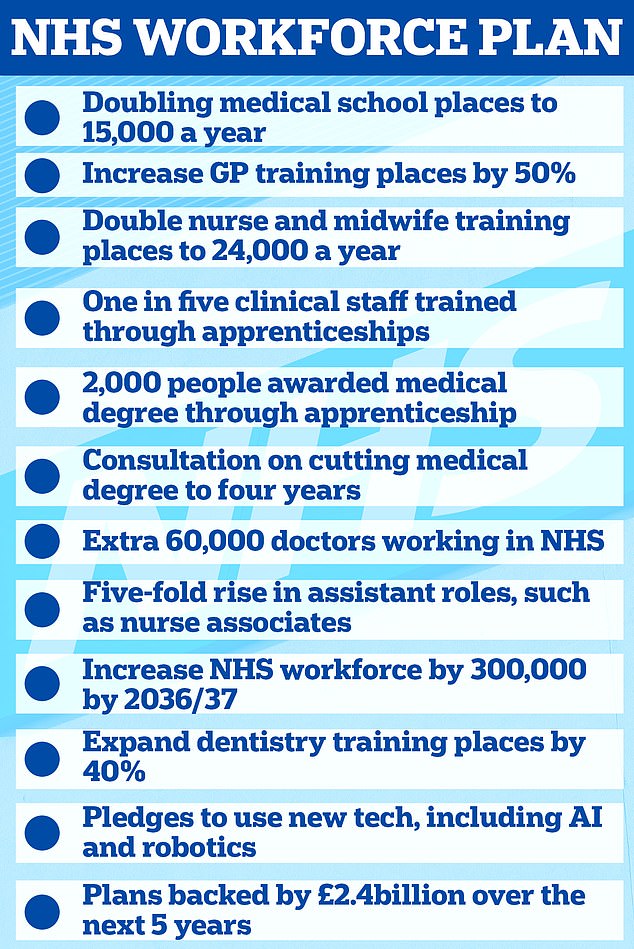
The proposals are detailed in the first NHS Long-Term Workforce Plan, which is published today and supported by £2.4billion of Government funding
The MP for Ilford North warned that the NHS ‘will die’ unless it adapts.
‘At the moment the NHS is in jeopardy. I’m anxious about the future of the NHS, as I think the rest of the country is,’ he told Sky News.
However, he rejected Sir Tony’s suggestion that Brits pay to access some services, saying: ‘I think we’ve already got a two-tier system in this country where people who can afford it are paying to go private and those who can’t are being left behind.’
Meanwhile, leading think tanks today warned that the NHS will not be around to celebrate its 100th birthday without more investment.
The King’s Fund, Health Foundation and Nuffield Trust said the NHS is the ‘jewel in the country’s crown’ but the service faces ‘huge challenges’.
In a letter to Prime Minister Rishi Sunak, and the leaders of the Labour and Liberal Democrat parties — Sir Keir Starmer and Sir Ed Davey — the organisations said the NHS has ‘endured a decade of underinvestment’.
Without action the service will face ‘managed decline that gradually erodes the guarantee of safety… it was designed to create’, they said.
The think tanks called for investment in the service, reform in the social care sector and action to address the ‘fraying health of the UK population’.
The letter states: ‘Seventy-five years after its creation, the National Health Service is in critical condition.
‘Pressures on services are extreme and public satisfaction is at its lowest since it first began to be tracked 40 years ago.
‘Despite this, public support for the NHS as an institution is rock solid — it still tops surveys about what makes people most proud to be British, and the public are unwavering in their support for its founding principles: free at the point of use, comprehensive and available to all.’
NHS Providers — which represents NHS acute, ambulance, community and mental health services — warned that the NHS faces ‘intense’ pressure and ‘the biggest financial squeeze in its history’ as it enters its 75th year.
Strikes, a lack of reform in social care, the size of the waiting list, a ‘financial squeeze’ and a rise in demand for emergency care is fuelling pressure on the system, it said.
Sir Julian Hartley, its chief executive, told Sky News: ‘The NHS is under intense pressure, that’s absolutely clear.
‘I’ve worked in the NHS 30 years and I think this is perhaps the most pressurised I’ve seen it in terms of all of the challenges, in terms of recovering from Covid.’
NHS England chief executive Amanda Pritchard admitted that the service faces ‘huge challenges’ and it will take ‘many years’ for waiting lists to recover.

Shadow Health Secretary Wes Streeting, who has backed using the private sector to bolster the NHS, echoed calls for reform to make the service sustainable for the long term

NHS England chief executive Amanda Pritchard admitted that the service faces ‘huge challenges’ and it will take ‘many years’ for waiting lists to recover
She told BBC Radio 4’s Today programme: ‘We’ve said right from the beginning, that the pandemic was going to be, you know, at least a five-year challenge.
‘So we’re on to that but we’re not stopping there – we’ve got to look to the long-term future; the work on prevention; on new technology or new treatments is just as important.’
Ms Pritchard added: ‘There’s a consensus I think that there is going to need to be continuous investment in the NHS.
‘But there’s also consensus that we’re going to need to keep reforming, keep changing, and that’s what the NHS has been doing for 75 years.
‘We’re no longer the NHS of TB, the iron lung, the cottage hospital. Now we’re genomic medicine, with virtual wards with blood tests for cancer.’
It comes as Health Minister Maria Caulfield today admitted that the record 7.4million waiting list for NHS treatment in England — up from around 4million before the pandemic — could increase further.
She told Sky News this morning: ‘To patients, what matters is how long they’re waiting. They’re not really worried about who else is on the waiting list.
‘They want to know when their procedure or operation is happening, and we’ve significantly reduced that delay. We’ve virtually eliminated a two-year wait.’
Challenged on the 7.4million figure, she said: ‘That probably will go up higher because we are offering more procedures.’
But ‘the length of time people are waiting for their procedures is actually going down and that’s what matters to patients’.
Latest NHS data shows that more than 7.42million patients in England — or one in eight people — were in the queue for ops like hip replacements in April.
This includes 370,000 people stuck in limbo for at least a year, often in pain.
Efforts to bring down the backlog have been hampered by strikes, with 648,000 appointments, procedures and operations rescheduled as a result of walkouts in England, since the first mass walkout of nurses started in mid-December.
Medics plan to take to picket lines again this month, with junior doctors planning to stage a five-day strike from July 13 to 18. Consultants, the most senior doctors in the NHS, are also planning action on July 20 and 21.
NHS England boss Ms Pritchard said patients are left ‘heartbroken’ when appointments and operations are postponed due to industrial action.
She said the strikes, which are ‘pretty much back-to-back’, will pose a ‘real challenge’ for the NHS.
Earlier this week, the British Medical Association (BMA) threatened to strike ‘until the next general election and beyond’ and warned that other doctor groups could also stage walkouts, including GPs.
‘We are now eight months into the most disruptive, most significant period of industrial action in our history,’ Ms Pritchard told BBC Radio 4’s Today programme.
‘That is now likely to get more challenging again, as we hit both junior doctors and consultants taking action.’
She said: ‘We work with everyone to try and make sure that in the course of industrial action, we are focused on keeping patients safe and minimising disruption.
‘But the hard truth is this is now proving to be really very disruptive for patients.’
Ms Pritchard urged the Government and unions to ‘redouble their efforts to find a solution’, noting that the NHS can’t afford to let strikes ‘drag on into this winter’.

