Sometimes women’s bodies function differently than men’s – sometimes with dramatic consequences.
You have to look closely to see what’s important – and the young cardiologist Margarethe Hochleitner did exactly that. When she looked around the intensive care unit of her hospital in the late 1970s, she noticed that almost all of the heart patients were men. “However, a look at the national statistics on causes of death revealed that cardiovascular diseases were also the biggest killer for women,” says Hochleitner today. She looked at the data on the care of patients with pacemakers. The result: It was mainly men who received the device to support their hearts.
“Of course you ask yourself what kind of illnesses these poor women have,” says Hochleitner, who worked for more than 15 years as a professor of gender medicine and director of the women’s health center at the Medical University of Innsbruck. “They don’t have to go to the intensive care unit, they don’t need a pacemaker, but in the end they die of a broken heart – it doesn’t add up.” Back in the late 1970s, she quickly realized that something was wrong with women’s medical care.
Hochleitner doesn’t want to accuse anyone of malice. “However, women’s hearts still have an awareness problem today,” says the doctor, who is now the training officer for gender medicine at the Austrian Medical Association. And that means: people look at things less closely. For much of the last century, heart disease was considered a men’s problem. After a life of heroic work, it was believed that it was her pumping muscle that eventually failed. The only role that was intended for women in this story was that of self-sacrificing caregivers. The American Heart Society even held a conference in the 1960s on “How can I help my husband cope with heart disease?” Back then, no one was interested in women’s hearts.

The US cardiologist Nanette Wenger (here 1981) is a pioneer of “gender-sensitive medicine”
© Fairfax Media via Getty Images / Getty Images
The male norm
After all, men were also the norm in medicine. Most drug information leaflets were based on studies of middle-aged white men. And even when women were later allowed to take part in clinical trials, it was rarely examined whether gender made a difference in the outcome.
The example of digoxin shows how dangerous this “one size fits all” approach can be. After American cardiologists had first certified the active ingredient’s convincing effectiveness in the treatment of heart failure in 1997, their conclusion had to be changed in a crucial point five years later. The study results had now been analyzed separately by gender. And it turned out that the drugs didn’t make women healthier – they actually died earlier. Other heart medications have also been found to cause more side effects in women, such as dangerous cardiac arrhythmias, or that they have to be dosed differently.
Demographic factor
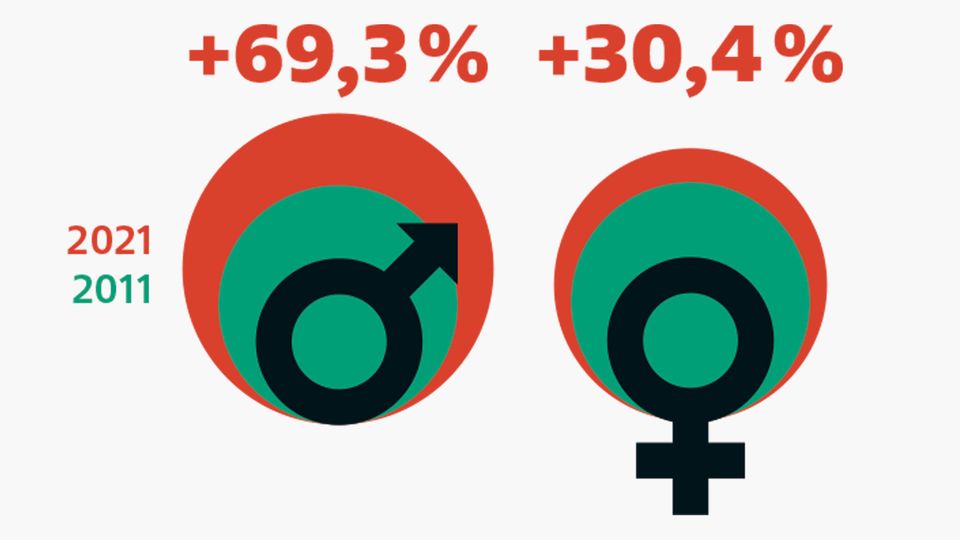
The change in the age composition of the population alone is causing an increase in heart diagnoses: from 2011 to 2021, the number of men aged 80 and over in Germany increased by 69.3 percent, and the number of women in this age group increased by 30.4 percent.
© Bettina Müller / star
However, even decades later, this knowledge has not yet reached everyone, says Margarethe Hochleitner, who has long been campaigning for more information. In Germany, the teaching of medical differences between the sexes has so far only been firmly integrated into the curriculum at very few universities. Many students hardly know anything about the topic. And women in the population also lack information.
The best example is heart attack, which does occur in women – but because of the protective effect of the female sex hormone estrogen, it often occurs later in life than in men. The symptoms can also be different. For decades, people have been trained to pay attention only to the annihilating pain in the chest that wrestles you to the ground in a Hollywood pose. “Women in particular often also – or only – complain of fatigue, vomiting, dizziness, upper abdominal pain or back pain,” says Viyan Sido, a specialist in cardiac surgery at the Asklepios Hospital in Hamburg. It’s not just the emergency services who may suspect that there are intervertebral disc or stomach problems. “Many patients also don’t know how to interpret their complaints – or downplay them because they don’t want to be a burden to anyone,” says Sido. The result: women with heart attacks come to the hospital later than men.
“I like to ask my students the question: Imagine an older woman lying on the sidewalk in Innsbruck – or an older man. What do you think is happening? When it comes to the man, the students immediately shout: Get an emergency doctor immediately, he could “Have a heart attack. People are discussing whether the woman has hypoglycemia or is having a circulatory collapse. That’s frustrating.”
Bikini medicine for women
This distortion effect, called “gender bias,” still influences medicine today – and not just in heart attacks. Women also have a disproportionately high risk of dying from a stroke, wrote Nanette Wenger in an article for an American journal in February of this year. The 93-year-old is still one of the most respected cardiologists and scientists in women’s health today. For decades she has been researching how women’s and men’s hearts differ. In the early 1990s she coined the term “bikini medicine” – because for a long time research on and for women focused only on breasts and reproductive organs. We still feel the lack of knowledge about women’s bodies today: Wenger writes that women are still less likely to be taken to hospital by the emergency services in the event of a stroke than men. They were less likely to receive the correct diagnosis. And they would be less likely to receive the drug that can dissolve a blood clot in the brain.
Diagnostics is a problem anyway, says Margarethe Hochleitner. For men, for example, bicycle ergometry is the gold standard for detecting coronary heart disease. “For women, however, the stress ECG often gives incorrect results.” Sometimes what is needed is a computer tomography of the coronary arteries or an MRI scan.
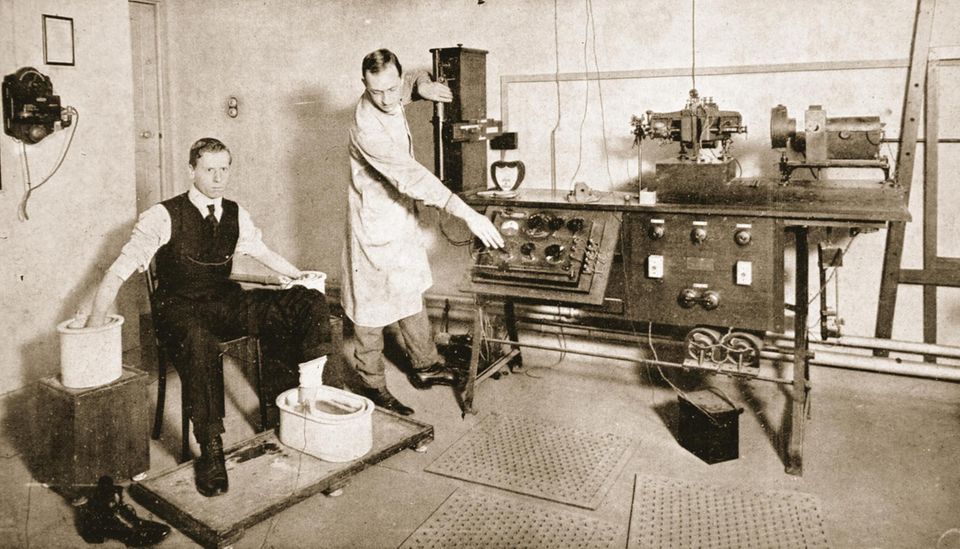
Heart examination of a prospective soldier at the beginning of the 20th century. Back then, it was hardly known that women also got heart disease
© Bridgeman Images
Basically, the list of inequalities starts with the risk factors. Women with diabetes mellitus have a higher risk of later developing heart failure than men. Smoking, autoimmune diseases and stress also seem to be more important for them than for men. Broken heart syndrome, for example, a dysfunction of the heart arteries caused by physical but also significant emotional stress, predominantly affects women. And what hardly any woman knows: If she suffers from high blood pressure during pregnancy, she has a two to four times higher risk of developing chronic high blood pressure a few years after giving birth. Even miscarriages are risk factors for later heart disease.
In the end, more women in Germany die from cardiovascular diseases than from cancer and lung disease combined. But not everyone is aware of this risk. So what advice can you give women? “Listen to your body,” says heart surgeon Sido. “Take your symptoms and your health seriously.” Women in particular often have the feeling that they cannot let go of their family and professional obligations. But in matters of the heart this can be life-threatening.