Pseudomonas aeruginosa is one of the most dangerous hospital germs in the world. The pathogen attacks the respiratory tract and lungs, which can be life-threatening for immunocompromised people.
Read more after the Advertisement
Read more after the Advertisement
A Swiss research group has now discovered how the bacteria gets into the lungs. The team cultivated lung organoids and then observed the sophisticated strategy the pathogen uses to break through the lungs’ defense line. The results were published in Journal “Nature Microbiology” published.
Bacteria penetrates natural protective barrier
The entire human respiratory tract is lined with a specialized mucous membrane that protects the deeper layers of the lung tissue. This mucous membrane consists of millions of cells with movable hairs, the so-called cilia, between which mucus-producing goblet cells sit.
Read more after the Advertisement
Read more after the Advertisement
Their mucus prevents microorganisms and thus pathogens from penetrating deep into the lungs. Instead, it forms an almost impenetrable barrier. Pseudomonas aeruginosa is, however, able to break through that barrier.
These bacteria are among the so-called hospital germs. According to the Robert Koch Institute They are one of the most common causes of pneumonia associated with hospital stays and are particularly life-threatening for immunocompromised and ventilated patients. World Health Organization (WHO) counts Pseudomonas aeruginosa among the twelve most dangerous bacterial pathogens in the world that are resistant to several antibiotics.
Researchers infect lung organoids
But how does the pathogen manage to penetrate the mucus barrier?
Clues are provided by lung organoids that the research group obtained from human stem cells and infected with the pathogen. “We have grown human lung microtissue that realistically mimics the infection process in a patient’s body,” Urs Jenal from the Biozentrum at the University of Basel is quoted as saying in a press release. “These lung models enabled us to uncover the pathogen’s infection strategy.”
Read more after the Advertisement
Read more after the Advertisement
A strategy from Greek mythology
In fact, the bacteria used a sophisticated strategy to penetrate the barrier tissue. The study describes this as follows: “In the first phase of infection, P. aeruginosa rapidly by using the nutrients available in the mucus layer.” In this initial phase, only a few bacteria come into contact with the tissue surface and the tissue remains intact.
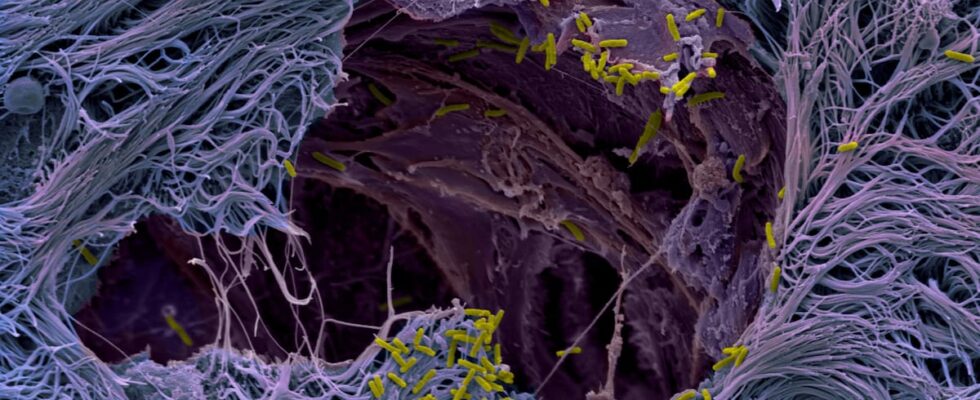
“In the next phase of the infection process, P. aeruginosato attach to and attack the underlying epithelial tissue, possibly because the mucus is exhausted, which is reflected in a halt in pathogen growth,” the study continues. The bacteria then used the mucus-producing goblet cells as Trojan horses. “By attacking the goblet cells, which make up only a small part of the lung mucosa, the bacteria can break through the line of defense and open the gate,” says Jenal.
Goblet cells burst and leave cracks
The pathogens attack the goblet cells with concentrated force, penetrate them, multiply and eventually cause the cells to burst and die. The bursting of the dead cells in turn leads to cracks in the barrier and thus to leaks, which are immediately exploited by the bacteria: they quickly settle in the weak spots, from where they spread into deeper tissue regions.
Read more after the Advertisement
Read more after the Advertisement
“Thanks to the development of human lung organoids, we now understand much better how pathogens behave in human tissue and presumably also in patients,” summarizes Jenal. Organoids of the human lung and other organs such as the bladder allow researchers to study the effects of antibiotics in tissue and, for example, determine where and how bacteria survive during treatment. They are therefore indispensable for the development of new and effective strategies to combat pathogens in the future.
RND/dpa