Status: 01/24/2023 12:07 p.m
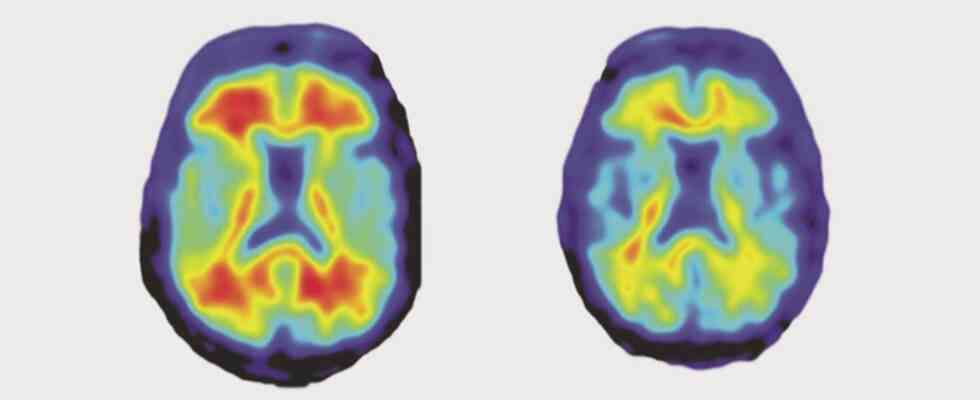
Viral infections can weaken the body in the long term, in rare cases chronic fatigue syndrome develops, possibly also dementia. A study finds evidence of a possible connection.
The analysis of 800,000 patient data in the specialist journal neuron shows a clear connection at first glance: people who survived a viral infection had a higher risk of suffering from neurodegenerative diseases such as dementia, Parkinson’s, Alzheimer’s or multiple sclerosis up to 15 years later. If people had pneumonia, severe flu or encephalitis, the risk of dementia was increased.
But what is the cause? Can previous viral infections really cause dementia? Or are patients with impaired brain functions simply more susceptible to viral infections overall? It is precisely these important questions that the study cannot answer. The research team only observed that people who have survived infections are more likely to develop dementia or Alzheimer’s – but what the cause is in each case cannot be deduced from such evaluations of patient data.
Do dementia patients get infected more often?
It may be that patients with dementia are more likely to contract viral infections overall – this could also be the reason for the connection observed in the study. There are indications that Alzheimer’s disease breaks out in the body 20 years before the first symptoms appear. However, the study only looks at the last 15 years. It is therefore possible that some patients are already suffering from dementia or Alzheimer’s unnoticed at the time of the virus infection, says neurobiologist Martin Korte from the TU Braunschweig: “At least in some people.”
An observation during the corona pandemic also speaks for this, says Korte: people who had Alzheimer’s disease before being infected have a higher risk of a severe course of Covid 19. At least it cannot be ruled out that Alzheimer’s patients have a weaker immune system overall and therefore have to fight infections more often.
Why viruses could cause dementia
However, there is also a lot to suggest that certain viral infections can actually weaken the brain in the long term, making neurodegenerative diseases such as dementia and Alzheimer’s more likely. This is shown by several studies with mice, says Korte: “We were already able to show in 2018 that a flu infection in particular also activates the immune system in the brain.” The neurobiologist suspects that microglial cells, i.e. the immune cells in the brain, could damage the nervous system for months.
“There is also data from the corona pandemic,” says Korte, referring to a study in the specialist journal Nature. Alzheimer’s patients had a particularly badly aged brain when they were struggling with a severe course of Covid 19. Also observed one science studythat infection with the Epstein-Barr virus can cause the neurological disease multiple sclerosis. Both studies provide evidence that viral infections can actually trigger neurodegenerative diseases. In dementia and Alzheimer’s patients, however, such a direct causal connection has not yet been observed.
Comparison between Finland and Great Britain
The study compares patient data from two different countries – Finland and the UK. Analysis of the Finnish data revealed 45 possible links between individual viral diseases and various neurodegenerative diseases such as dementia and Alzheimer’s.
When comparing the data from Great Britain, however, only 22 of the 45 connections were confirmed, says neurologist Klemens Ruprecht from the Charité in Berlin: “This suggests that some of the associations described could be false positive associations.” This means that the connections still have to be confirmed in further studies.
Vaccinations could reduce risk
If previous viral infections actually increase the risk of neurological diseases such as dementia and Alzheimer’s, vaccinations such as against influenza or shingles could become even more important, the research team writes in the study.
But it’s still too early for that, says virologist Klaus Überla from the University Hospital Erlangen: “Now it would be important to show that vaccinations reduce the frequency of neurodegenerative diseases.” Then the results would have to be checked carefully.
Research into causes before vaccination recommendations
For such preventive measures, however, it must first be clearly shown whether and how viral infections trigger dementia or Alzheimer’s in the first place. “The study is an important impetus for further research in this direction,” says Überla. So far, however, there have been no direct consequences for vaccination recommendations.